Who Will Care for America’s Seniors?
April 27, 2015 — by Alana Semuels • theatlantic.com

Lynne Sladky / AP
Being a home-health aide is a lonely, difficult job, and the pay is miserable. But the country needs to find millions more people to do it.
My grandfather broke his hip at age 87. At the time, he lived with my grandmother in western Massachusetts in a beautiful house they’d built themselves abutting a farm. At 88, she was as “with it” as someone decades her junior, and she was determined to help him continue to live at home, where he could listen to classical music in his sunny study, or gaze at the sheep that sometimes grazed outside his window.
He went to a nursing home for short-term rehab right after the accident, and it was nightmarish, she told me. He was trapped in a room with patients who would be there for the rest of their lives, which depressed him. Nurses gave him his medication on an erratic schedule, not necessarily prioritizing his health. My grandmother decided he would do better at home.
It didn’t seem like it would be too hard. They’d added a downstairs bedroom and bathroom a few years back, so he wouldn’t have to go up stairs. And she was still mobile, and could cook for him and spend time with him and set reminders on her iPad for when it was time for him to take his medication. She had family and friends nearby, who could spell her from caretaker duties from time to time. Plus, they had paid tens of thousands of dollars for long-term care insurance, which would pay for a home-care aide to come and help them when needed.
But finding help proved nearly impossible. The long-term-care insurer would only work with two agencies in the area, and they were swamped with demands. Often my grandmother would call and request help and no one could come. The agencies’ staff tended not to live in Amherst, a college town with a population of 35,000, and would have to come from other towns, driving a long way from one client to another.
In western Massachusetts, where unemployment is low and full-time steady work isn’t too hard to find, working a few hours a day for different clients for low pay didn’t appeal to many people. My grandmother didn’t need someone to be at the house all day. She mostly needed help getting my grandfather out of bed in the morning—he was a tall man, and was suffering from Parkinson’s disease, which meant his body sometimes wouldn’t obey his mind— into and out of the shower, and out of his wheelchair into bed at night. Though the agency charged $25 an hour, the workers only got about $15, which was, in fact, high for the field. The agency set a minimum visit of two hours, more than my grandparents needed at any one time.
Eventually, my grandmother stopped depending on the agencies, and, through a friend of a friend, found a Ph.D. student from Kenya named John. John was vastly overqualified for the job, but he was looking for a little extra cash, so he came to help my grandfather get out of bed in the morning and back into it at night, all while juggling his studies and his small family, who had moved with him to Amherst. John quickly became adept at the tasks of a home health aide, and he and my grandfather shared a bond, talking about Kenya and public health and academia. John was there when my grandfather suddenly died two years ago. My grandmother gave a donation to his village in his name as thanks for his help. She’s never heard from him again.
My grandparents lived in Amherst for 50 years. They didn’t want to move as they got older, and they weren’t unusual in this. Nearly 90 percent of seniors want to stay in their own homes as they age, according to AARP. Sometimes, it’s not a choice: Government programs such as Medicaid, in an effort to save money, are shifting spending away from institutional settings toward home and community-based care.
At the same time, the number of seniors is growing. In 2010, one-sixth of the adult U.S. population was older than 65; by 2030, about one-fourth will be.
“What’s coming down the pipeline—it’s a demographic tsunami,” Lawrence Force, director of the Center on Aging and Policy at Mount Saint Mary College, told me.
But the resources to help seniors stay at home are shrinking. Many seniors are finding that their boomer children are staying in the workforce longer than they did, and are unable to care for them. Demand for direct-care workers is expected to grow 37 percent between 2012 and 2022. Demand for personal care aides alone—the entry-level workers in the field—will grow 49 percent. There are currently 3.5 million direct-care workers in the country, according to the Bureau of Labor Statistics. Seven years from now, there will be 1.3 million more.
More and more people are going to face the same problem my grandparents faced. They may have saved lots of money, or bought into long-term care insurance, and they might have all their affairs in order. But that doesn’t mean they’re going to be able to find someone to take care of them when they stay at home. About 20 percent of the elderly live in non-metropolitan designated areas, according to the National Rural Health Association, which makes it harder for them to find helpers nearby.
Money is also a problem: Medicaid reimbursement rates govern wages in the industry, but states have kept reimbursements flat as they struggle with budget issues, said Abby Marquand, Director of Policy Research with the Paraprofessional Healthcare Institute, or PHI. It’s part of the Catch-22 of the home-care aide field—policymakers want to help people age at home because it’s cheaper than a nursing home, but agencies argue that it won’t be cheaper anymore if they raise wages and pay for overtime.
The resulting dearth of workers who stick with the field is creating headaches for the agencies charged with caring for the elderly at home.
“We can’t find quality staff—I can hire 10 people and keep two,” Jacqui Carson, the chief executive of Sanborn Place Home Care and Day Services, a residence for low-income seniors in the Boston area that also provides home care, told me. “This job doesn’t pay, because reimbursements are low.”
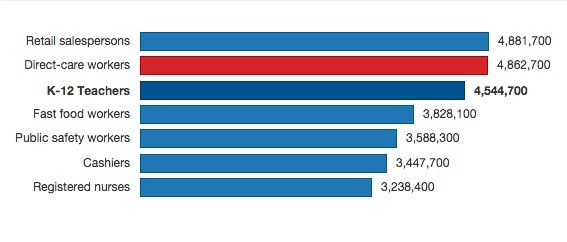
Source: Bureau of Labor Statistics, Paraprofessional Healthcare Institute
Carson’s organization also runs a home-care service, and during the snowstorms this winter, staff couldn’t get to patients’ homes, and, even if they could, they couldn’t afford child care for their kids who were home with snowdays. So Carson shoveled her way into seniors’ houses herself.
To get more dedicated people in the field, though, something needs to change, she said.
“I would hope that somewhere along the way, people understand that our CNAs are as needed as our engineers,” she said.
Part of the problem is the very nature of the jobs. On average, home care aides work 34 hours a week, and make an average of $17,000 a year. One in four live in households below the federal poverty line, and one in three doesn’t have health care because their employer doesn’t offer it or because they can’t afford it. Perhaps unsurprisingly, the field has a high rate of turnover—some estimates put it as high as 60 percent.
Of the ten occupations that added the most new jobs in 2012, personal-care aides earned less than all except for fast-food workers, according to the Paraprofessional Healthcare Institute.
“Some would call it a dead end job,” said Deane Beebe, a spokeswoman for the Paraprofessional Healthcare Institute, or PHI. “These are very hard jobs. They’re very physically taxing—they have one of the highest injury rates of any occupation—and they’re very emotionally taxing: It’s intimate work; it’s isolating work.”
There are efforts under way to make these jobs more appealing to workers, but they haven’t gained much traction yet.
For one thing, home care aides aren’t covered included under the Fair Labor Standards Act, which means they’re not subject to overtime pay or minimum wage requirements. The Obama Administration extended the FLSA in 2013 to cover home-care workers, but a federal judge struck down that rule in January of this year. The Department of Labor is appealing the ruling, which applies to home care aides and personal care assistants, but not nursing assistants.
At the core of the debate is whether America’s 1.7 million home-care aides are “elder sitters,” and are thus, like babysitters, excluded from labor rules. Congress expanded FLSA coverage to domestic service workers in 1974, but exempted babysitters and companions for the aged and infirm. In his decision, the federal judge wrote that Congress would have to change the law in order to include home care aides under the labor standards—it currently likens aides to babysitters, he wrote.
In an amicus brief, dozens of members of Congress argued that the field had changed dramatically since 1974, and that home-care aides should be covered under the FLSA.
“The home-care labor force is not what it was in 1974,” the brief said. “The entire enterprise has changed into a professionalized workforce that is exactly the type Congress intended that FLSA cover.”

Lynne Sladky/AP
If home-care workers were treated as professionals, rather than “elder sitters,” some advocates argue, receiving better pay and benefits and stable hours, it would be easier to attract workers to the field and to retain them. In addition, a nationwide training system could also help prepare workers for the challenges of helping the sick and infirm, which would also reduce turnover.
“Turnover is related to a lack of training as well as a lack of career advancement opportunities,” said Leanne Winchester, the project director for Direct Care Workforce Development, a program being run by UMass Medical School and the state of Massachusetts.
Though some states have training requirements, there is currently no federal standard for training or assessment of personal-care aides, which is an entry-level position in the field. Some states, including California and Iowa, have no training requirements at all. Many workers become personal care aides because they need a job and because someone—like my grandmother—is desperate for help, right away. They find the job on Craigslist and it seems like an easy way to make money, and then they run into obstacles—they’re not prepared to work with someone who has had a stroke, or to be in an environment that might have bed bugs— and they quit, said Lisa Gurgone, the executive director of the Home Care Aide Council.
Gurgone and others are advocating for more training for workers, which will prepare them for working in the field. As part of the Affordable Care Act, six states have piloted programs to train and evaluate the direct care workforce. Some of those programs, including the one in Massachusetts, included what’s called a “career lattice,” which allows workers to move laterally along a career path by developing specialized skill sets. The goal is that by acquiring different skill sets, they can then move up the career ladder into higher-paying jobs.
This was the first recommendation agreed upon by the Commission on Long-Term Care, which was tasked with coming up with recommendations as to how to best provide and pay for long-term care.
“Direct care worker positions are often viewed as low-wage, entry-level jobs with little to no opportunity for advancement,” the Commission’s report to Congress says. “Establishing career ladders and lattices can increase the desirability of these positions, and improve job retention.”
I took a look at what this training might look like when I stopped by a class in Lynn, Massachusetts, for home-health aides, being run by All Care VNA and Hospice. All Care had posted ads on Craigslist saying it would train workers and then find them jobs, and many of the people in the room had come from other fields, eager to join a fast-growing profession.
“It’s a field that’s just going to keep growing and growing,” one student, Stephanie Rodriguez, told me. Rodriguez had previously worked in fast food and as a receptionist, but said she thought being a home-care aide would give her more flexibility to spend time with her family.
She sat at a long table with a dozen other students, all of whom were minorities. They had binders out and were taking notes when I walked in, watching a video that talked about proper techniques for bathing elders. The previous day, they’d gone over nutrition and planned some meals for would-be clients. Conversation had veered to cleanliness in seniors’ homes, and they learned to keep all their personal belongings in their car to avoid bed bugs, and to wear booties if there was a risk of infection. Later in the week, they’d practice “transfers”—helping seniors out of their wheelchairs and into bed or onto the toilet.
The training was based on the PHCAST curriculum, and seemed much more extensive than any of the quick babysitting prep talks I’ve ever heard, and I couldn’t help but wonder how people would fare in the field without getting this sort of instruction first.
Gurgone told me the training is useful in weeding out people who just want quick money but who won’t be reliable. One student who was going through the training learned about the possibility of a client having bed bugs, and quit then and there.
“These workers, they need jobs,” Gurgone told me. “But the people who succeed in this job, they do it because it’s like a calling.”

Tony Dejak/AP
Many of the students in the room said they were testing out the field, and if they liked it, they’d perhaps trying to become nursing assistants or go to school for other jobs in the healthcare field. It was what drew some of them from other fields: After all, there are many low-wage jobs out there, but most workers won’t find opportunities for promotion and further schooling in fast food restaurants.
Rodner Chery, for example, had worked in the kitchen of a nursing home for a decade, but wanted to do something different, he said.
“When you’re working in the kitchen, especially if you don’t want to be there, you’re stuck and you don’t want to be,” he said. “Here, they let me do something different, and I can grow. I know the field is huge.”
No matter how much training workers receive, though, it’s unlikely that they’re going to stay on the job unless they can afford to do so. For this to change, states need to put more money into Medicaid, said Marquand, of PHI. But the opposite is currently happening. States including Connecticut, California and Illinois are planning to cut back on eligibility of Medicaid recipients and are requiring low-income seniors to pay more for their care as a way to close budget gaps.
Workers won’t likely get help from their employers either: It was the associations representing home-care agencies that filed the lawsuit against the Department of Labor asking that workers not receive minimum wage or overtime.
Had the Department of Labor rule gone into effect January 1st of this year, as scheduled, “it will have a destabilizing impact on the entire home care industry,” argued the plaintiffs, Home Care Association of America, the International Franchise Association and National Association for Home Care and Hospice (PHI argues that the $100 billion industry can afford to pay its workers a little more).
Some workers have unionized in an effort to force change in the field. This often begins with states recognizing independent home-care workers funded by Medicaid as public employees, which allows them to organize, as happened in Oregon, California and Washington. Home-care associations in Pennsylvania are battling an executive order by newly elected Gov. Tom Wolf that could make it easier for home-care workers to unionize. Lawmakers in Minnesota passed a bill last year allowing these independent home-care workers to be represented by unions, as did lawmakers in Connecticut in 2012 . After Vermont passed a similar bill, home-care workers there unionized too, as I wrote about this fall.
There is some proof that unionizing can raise standards: Ten years after Illinois approved a union for home healthcare workers, wages doubled and training and standards improved, according to NPR. The Vermont workers I talked to mentioned time and the significance of being in a union. Their jobs are isolating and stressful, but having others to talk to and advocate with has made a difference, they said. What’s more, as union members, they are able to advocate for their clients, protesting against cuts in state Medicaid payments and services.
“For a long time, we were just employees of someone—an agency, the state,” one worker, Amanda Sheppard, told me. “Now, we are being advocates and liaisons for our clients in the state.”
Of course, depending on unionization to improve life for home-care workers isn’t an easy fix, either. Last year, the Supreme Court ruled that home-care workers in Illinois cannot be required to pay unions fees if they’re not in a union, categorizing the workers as “quasi-public employees”—not “babysitters,” but not what advocates for home-care workers had wanted, either.
Read the article here:
http://www.theatlantic.com/business/archive/2015/04/who-will-care-for-americas-seniors/391415/
About the Author

ALANA SEMUELS is a staff writer at The Atlantic. She was previously a national correspondent for the Los Angeles Times.
Follow her on Twitter


Follow Us!